Connect With Us

Plantar Fasciitis
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk for developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.
Custom Orthotics Can Be Used In Stylish Footwear
Who said style can't be comfortable? With Custom Orthotics, you get the best of both worlds. Slip them into your favorite fashionable shoes and feel the difference. They mold to your feet, offering support without compromising on style. No more choosing between looking good and feeling great. With Custom Orthotics, step out in style and comfort every day. Contact our office to learn more!
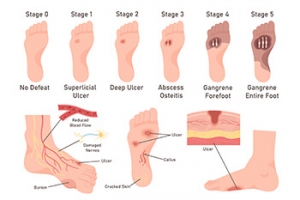
Debridement Methods for Diabetic Foot Ulcers
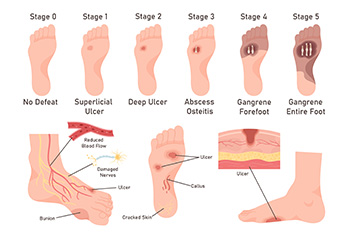
Debridement is a key procedure in managing diabetic foot ulcers, involving a podiatrist removing dead and infected tissue to promote healing and prevent infection spread. This process is vital because the buildup of necrotic tissue can obscure the true extent of the ulcer. There are several methods of debridement. Surgical debridement involves a podiatrist using tools like scalpels to precisely remove dead tissue, often performed at the bedside or in an operating room for more severe cases. Mechanical debridement employs saline-soaked pads that adhere to and remove dead tissue upon removal, though this can be painful and may also disturb healthy tissue. Chemical debridement uses enzymes to dissolve dead material. Biological debridement, utilizing maggots, effectively cleanses wounds by consuming only dead tissue. Before any debridement, the podiatrist will assess the patient’s overall health, and the wound will be cleaned with a saline solution. If you have diabetic foot ulcers, it is suggested that you make a podiatrist a part of your medical team for expert wound care options.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Dr. Eddy Caldwell from Foot Care of Northeast Arkansas, P.A.. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Jonesboro, AR . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Custom Orthotics for Those With Diabetic Foot Ulcers
 Custom orthotics for individuals with diabetes and foot ulceration are specialized devices designed to provide optimal support and protection for feet at high risk of complications. Diabetic feet are prone to neuropathy and poor circulation, making them vulnerable to ulcers and infections. Custom orthotics are meticulously crafted to fit the unique shape and pressure points of the patient’s feet, offering targeted relief and reducing pressure on ulcer-prone areas. These orthotics help by redistributing weight evenly across the foot, minimizing friction and pressure that can cause or exacerbate ulcers. They also provide cushioning to absorb shock and reduce the risk of injuries. The precise fit of custom orthotics ensures that there are no areas of excessive pressure, which is imperative in preventing further complications. The fitting process for custom orthotics involves a thorough examination by a podiatrist, who may use techniques like 3D scanning or casting to create an accurate model of the foot. This ensures that the orthotic device is tailored specifically to the patient's needs, providing maximum protection and comfort. If you are a diabetic with foot ulcers, it is strongly suggested that you make an appointment with a podiatrist to discuss custom-made orthotics to provide relief.
Custom orthotics for individuals with diabetes and foot ulceration are specialized devices designed to provide optimal support and protection for feet at high risk of complications. Diabetic feet are prone to neuropathy and poor circulation, making them vulnerable to ulcers and infections. Custom orthotics are meticulously crafted to fit the unique shape and pressure points of the patient’s feet, offering targeted relief and reducing pressure on ulcer-prone areas. These orthotics help by redistributing weight evenly across the foot, minimizing friction and pressure that can cause or exacerbate ulcers. They also provide cushioning to absorb shock and reduce the risk of injuries. The precise fit of custom orthotics ensures that there are no areas of excessive pressure, which is imperative in preventing further complications. The fitting process for custom orthotics involves a thorough examination by a podiatrist, who may use techniques like 3D scanning or casting to create an accurate model of the foot. This ensures that the orthotic device is tailored specifically to the patient's needs, providing maximum protection and comfort. If you are a diabetic with foot ulcers, it is strongly suggested that you make an appointment with a podiatrist to discuss custom-made orthotics to provide relief.
Experience a transformative solution to heel pain and foot pain through the personalized benefits of custom orthotics and shoe inserts. If you’re grappling with the persistent agony of plantar fasciitis, these customized inserts are designed to alleviate the strain on the plantar fascia, providing targeted relief. Engineered to adapt to your unique foot anatomy, custom orthotics tackle not only plantar fasciitis but also general foot and heel pain, offering unparalleled support and comfort. Don’t let every step be a reminder of discomfort; step into a world of tailored well-being. Say farewell to the limitations imposed by heel pain and embrace the freedom of pain-free mobility. Invest in your foot health and redefine your daily stride with the transformative power of custom orthotics and shoe inserts, ensuring each step is a step towards lasting comfort.
If you have any questions please contact our office located in Jonesboro, AR . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Investing in Custom Orthotics Means Investing in Foot Health
Custom orthotics offer a tailored approach to foot health, providing a host of benefits that extend far beyond conventional shoe inserts. One of the primary advantages lies in their ability to address specific biomechanical issues. Unlike off-the-shelf inserts, custom orthotics are crafted based on an individual's unique foot structure, gait, and any existing foot conditions.
The personalized design of custom orthotics ensures optimal support for the arches, promoting proper alignment and distributing pressure evenly across the feet. This can be particularly beneficial for individuals dealing with issues such as overpronation or underpronation, as custom orthotics help correct imbalances that may lead to discomfort or injury.
Beyond biomechanics, custom orthotics can alleviate a range of foot problems, including plantar fasciitis, bunions, and metatarsalgia. They provide targeted relief to areas under stress, reducing pain and inflammation. Additionally, for those with specific medical conditions like diabetes, custom orthotics can play a crucial role in preventing complications associated with poor foot health.
Comfort is another key aspect of custom orthotics. By accommodating the unique contours of an individual's feet, these inserts enhance overall comfort, making daily activities more enjoyable. Whether for athletes looking to optimize performance or individuals seeking relief from chronic foot pain, custom orthotics offer a versatile solution.
Investing in custom orthotics is an investment in long-term foot health. They not only provide immediate relief but also contribute to the prevention of future issues. With the ability to seamlessly integrate into various types of footwear, custom orthotics empower individuals to prioritize foot comfort without compromising on style. In essence, custom orthotics are a personalized prescription for happy, healthy, and pain-free feet.
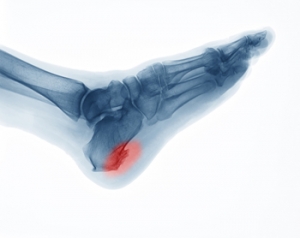
Causes and Definition of Heel Spurs
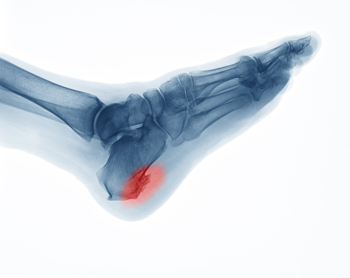 A heel spur, medically known as a calcaneal spur, is a bony growth that develops on the underside of the heel bone. This condition often results from long-term strain on the foot muscles and ligaments, commonly associated with repetitive activities such as running or jumping. Over time, this strain leads to the accumulation of calcium deposits, forming the bony protrusion. Heel spurs are frequently linked to plantar fasciitis, an inflammation of the plantar fascia tissue that runs along the bottom of the foot. Factors contributing to heel spur development include wearing ill-fitting shoes, excessive weight, and having flat feet or high arches. If you have heel pain, it may be indicative of a heel spur, and it is suggested that you consult a podiatrist who can accurately diagnose and offer a comprehensive treatment plan for heel spurs.
A heel spur, medically known as a calcaneal spur, is a bony growth that develops on the underside of the heel bone. This condition often results from long-term strain on the foot muscles and ligaments, commonly associated with repetitive activities such as running or jumping. Over time, this strain leads to the accumulation of calcium deposits, forming the bony protrusion. Heel spurs are frequently linked to plantar fasciitis, an inflammation of the plantar fascia tissue that runs along the bottom of the foot. Factors contributing to heel spur development include wearing ill-fitting shoes, excessive weight, and having flat feet or high arches. If you have heel pain, it may be indicative of a heel spur, and it is suggested that you consult a podiatrist who can accurately diagnose and offer a comprehensive treatment plan for heel spurs.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Dr. Eddy Caldwell from Foot Care of Northeast Arkansas, P.A.. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our office located in Jonesboro, AR . We offer the latest in diagnostic and treatment technology to meet your needs.
Heel Spurs
Heel spurs are the result of calcium deposits that cause bony protrusions on the underside of the heel. Heel spurs are usually painless, but they have the potential to cause heel pain. Heel spurs tend to be associated with plantar fasciitis, which is a condition that causes inflammation of the band of connective tissue that runs along the bottom of the foot. They most often occur to athletes whose sports involve a lot of running and jumping.
Some risk factors for developing heel spurs include running and jogging on hard surfaces, being obese, wearing poorly fitting shoes, or having walking gait abnormalities.
It is possible to have a heel spur without showing signs of any symptoms. However, if inflammation develops at the point of the spur’s formation, you may have pain while walking or running. In terms of diagnosis, sometimes all a doctor needs to know is that the patient is experiencing a sharp pain localized to the heel to diagnose a heel spur. Other times, an x-ray may be needed to confirm the presence of a heel spur.
Heel spurs can be prevented by wearing well-fitting shoes that have shock-absorbent soles. You should also be sure that you are choosing the right shoe for the activity you want to partake in; for example, do not wear walking shoes when you want to go on a run. Additionally, maintaining a healthy weight can be beneficial toward preventing heel spurs, as it will prevent an excess amount of pressure being placed on the ligaments.
There are a variety of treatment options for people with heel spurs. Some of these include stretching exercises, physical therapy, shoe inserts, or taping and strapping to rest stressed muscles and tendons. If you have heel pain that lasts longer than a month, don’t hesitate to seek help from a podiatrist. Your doctor can help you determine which treatment option is best for you.
Lifestyle Factors and Medical Reasons for Cracked Heels

Cracked heels are caused by various lifestyle factors and medical reasons. Prolonged standing, wearing open-backed shoes, and walking barefoot on hard surfaces can contribute to the development of dry, cracked skin on the heels. Medical conditions such as diabetes, thyroid disorders, and eczema can also lead to cracked heels by causing dryness and reducing the skin's natural elasticity. To help prevent cracked heels, apply a thick, hydrating lotion to keep the feet moisturized. Wearing supportive, closed-back shoes can help reduce pressure on the heels. Additionally, using a pumice stone to gently exfoliate dead skin and avoiding walking barefoot on hard surfaces can be beneficial. If you have developed cracked heels, it is suggested that you consult a podiatrist who can effectively treat this condition, which may include prescribed medicine.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact Dr. Eddy Caldwell from Foot Care of Northeast Arkansas, P.A.. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
- Invest in a good foot cream
- Try Using Petroleum Jelly
- Ease up on Soaps
- Drink Plenty of Water
Ways to Prevent Cracked Heels
- Moisturize After Showering
- Skip a Shower
- Keep Shower Water Lukewarm
- Don’t Scrub Your Feet
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact our office located in Jonesboro, AR . We offer the newest diagnostic and treatment technologies for all your foot care needs.