Connect With Us

Key Facts About Plantar Warts

Plantar warts are small, hard growths that appear on the bottom of the feet, often on the heel or the ball of the foot. They are caused by the human papillomavirus, or HPV, which enters the skin through tiny cuts or abrasions. While these warts are generally harmless, they can be painful, especially when pressure is applied while standing or walking. Plantar warts are contagious and can spread from person to person, typically in damp, warm environments like public showers or swimming pools. These warts often appear as rough, thickened areas of skin with tiny black dots, which are small blood vessels. Although they may go away on their own, plantar warts can take months or even years to disappear. Relief options include mild removal applications, cryotherapy, or in some cases, surgical removal. Plantar warts can cause pain and discomfort, and may lead to difficulty in completing daily activities. If you have developed this condition, it is suggested that you promptly contact a podiatrist who can offer you effective treatment and relief solutions.
Plantar warts can be very uncomfortable. If you need your feet checked, contact Dr. Eddy Caldwell from Foot Care of Northeast Arkansas, P.A.. Our doctor will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our office located in Jonesboro, AR . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What Are Plantar Warts?
Plantar warts are described as small growths that appear on the heels or other areas of the feet that bear a large amount of weight. The pressure in these areas causes plantar warts to hide behind thick layers of skin called calluses. In most cases, plantar warts are not a serious health issue, and they usually go away without treatment. However, it is still important be mindful of them.
Plantar warts are caused by infections with human papillomavirus (HPV) in the outer layer of skin on the soles of the feet. The plantar warts then develop when the virus enters the body through weak spots at the bottom of the feet, such as tiny cuts and breaks. Plantar warts are not guaranteed for all who encounter the virus. Everyone responds differently to the affects of HPV.
Plantar warts are most common in the following groups: children and teenagers, people with weakened immune systems, people with history of plantar warts, and people who walk barefoot. Exposure to HPV is common in environments such as locker rooms or pool areas.
One of early signs to look out for is a callus, since many plantar warts hide behind them. You can also locate these warts by looking for small, fleshy, rough, grainy growths near the base of the toes and the heel. Early signs of plantar warts are shown by black pinpoints, which are small, clotted blood vessels. Lesions that interrupt normal lines and ridges in the skin of your foot may also be a sign of plantar warts. Any feeling of pain while walking or standing can also be a symptom of plantar warts.
Although most cases are not serious, some conditions may require a visit to your podiatrist. If you are uncertain that your lesion is a wart, if you have diabetes, or if you are experiencing bleeding, you may need to see a seek professional treatment. Your doctor may offer treatments such as prescribing stronger peeling medicine or using cryotherapy by applying liquid nitrogen to the wart. More serious cases may require minor surgery or laser treatment.
There are simple solutions available to help prevent plantar warts. One common task is to avoid walking barefoot in swimming pool areas and locker rooms, as this is where HPV is commonly present. Keeping your feet clean and dry, while changing shoes and socks daily can also help prevent future plantar warts. If you know someone who has plantar warts, it is important to avoid direct contact with their warts. You should also refrain from picking or scratching your wart if you happen to develop one.
How Seniors Can Benefit from Foot Orthotics

Foot orthotics offer significant benefits to seniors, particularly in preventing falls and improving balance. As people age, foot health can decline leading to issues like weakened arches, poor alignment, and discomfort. These conditions can contribute to instability and increase the risk of falls. Custom-made foot orthotics help by providing necessary support, stabilizing the feet, and ensuring proper alignment, which enhances overall balance and posture. By redistributing pressure across the foot, orthotics reduce the strain on joints and muscles, allowing for smoother and more confident movements. Proper foot support helps seniors maintain their posture while walking, reducing the likelihood of stumbling or losing balance. For seniors with conditions like arthritis, flat feet, or diabetes, orthotics provide pain relief and improve mobility. Foot orthotics help seniors move with greater stability and reduce the risk of falling. If you are a senior experiencing foot or ankle pain, it is suggested that you consult a podiatrist to determine if orthotics are right for you.
If you are experiencing discomfort in your feet and would like to try custom orthotics, contact Dr. Eddy Caldwell from Foot Care of Northeast Arkansas, P.A.. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Are Custom Orthotics?
Custom orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain.
Over-the-Counter Inserts
Shoe inserts come in a wide variety and are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality, custom inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you're experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibility of using custom orthotics or shoe inserts. A podiatrist can determine which type of custom orthotic or shoe insert is right for you and help you take the first steps toward being pain-free.
If you have any questions please contact our office located in Jonesboro, AR . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Investing in Custom Orthotics Means Investing in Foot Health
Custom orthotics offer a tailored approach to foot health, providing a host of benefits that extend far beyond conventional shoe inserts. One of the primary advantages lies in their ability to address specific biomechanical issues. Unlike off-the-shelf inserts, custom orthotics are crafted based on an individual's unique foot structure, gait, and any existing foot conditions.
The personalized design of custom orthotics ensures optimal support for the arches, promoting proper alignment and distributing pressure evenly across the feet. This can be particularly beneficial for individuals dealing with issues such as overpronation or underpronation, as custom orthotics help correct imbalances that may lead to discomfort or injury.
Beyond biomechanics, custom orthotics can alleviate a range of foot problems, including plantar fasciitis, bunions, and metatarsalgia. They provide targeted relief to areas under stress, reducing pain and inflammation. Additionally, for those with specific medical conditions like diabetes, custom orthotics can play a crucial role in preventing complications associated with poor foot health.
Comfort is another key aspect of custom orthotics. By accommodating the unique contours of an individual's feet, these inserts enhance overall comfort, making daily activities more enjoyable. Whether for athletes looking to optimize performance or individuals seeking relief from chronic foot pain, custom orthotics offer a versatile solution.
Investing in custom orthotics is an investment in long-term foot health. They not only provide immediate relief but also contribute to the prevention of future issues. With the ability to seamlessly integrate into various types of footwear, custom orthotics empower individuals to prioritize foot comfort without compromising on style. In essence, custom orthotics are a personalized prescription for happy, healthy, and pain-free feet.
Symptoms and Treatment of Bunions

A bunion is a bony enlargement that develops at the base of the big toe, often caused when the top of the toe angles toward the others. This misalignment can lead to pain, swelling, redness, and difficulty walking. Other symptoms include irritated skin over the bump or stiffness in the joint. Bunions can develop due to genetics, foot structure, or wearing shoes like high heels that squeeze the toes or shift weight toward the forefoot. Bunions are diagnosed through physical examination, questions about symptoms and footwear, and sometimes X-rays to assess the joint’s alignment. Treatment focuses on reducing discomfort and improving foot function. A podiatrist can recommend footwear that minimizes pressure, as well as prescribe orthotic devices like splints or pads to improve alignment and provide cushioning. In more severe cases, this foot doctor may discuss surgery to restore joint alignment. If you have a problematic bunion, it is suggested that you schedule an appointment with a podiatrist for a diagnosis and treatment options.
If you are suffering from bunion pain, contact Dr. Eddy Caldwell of Foot Care of Northeast Arkansas, P.A.. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our office located in Jonesboro, AR . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What Are Bunions?
Bunions are large bony bumps at the base of the big toe. Medically known as hallux valgus, a bunion is a misalignment of the metatarsophalangeal joint, or big toe joint. The misalignment will generally worsen with time if left untreated.
The exact cause of bunions is unknown, with genetics seen as a potential cause. High heels and poorly-fitted footwear, rheumatoid arthritis, and heredity all seem to be potential factors behind the exacerbation of bunions. Women have been found to be more likely to develop bunions in comparison to men.
Bunions do not always produce symptoms. The best way to tell is if the big toe is pushing up against the next toe and there is a large protrusion at the base of the big toe. You may or may not feel pain. Redness, swelling, and restricted movement of the big toe may be present as well.
Podiatrists use a variety of methods to diagnose bunions. If there are symptoms present, podiatrists will first consider that it is a bunion. If not, a physical examination will be conducted to check function of the big toe. Finally, an X-ray may be taken to view the extent of the bunion and confirm it is a bunion.
Typically, nonsurgical methods are used to treat bunions, unless the bunion has become too misaligned. Orthotics, icing and resting the foot, roomier and better fitted shoes, taping the foot, and pain medication are usually utilized first. If the bunion doesn’t go away or causes extreme pain, surgery may be required. Surgeons will either remove part of the swollen tissue or bone to straighten the toe out.
If you have a bunion, it is recommended to see a podiatrist. The longer it is left untreated, the worse it may get. Podiatrists can properly diagnose and treat a bunion before it gets worse.
Keep Your Feet Healthy So You Can Stay Active
Dangers of Chronic Tophaceous Gout
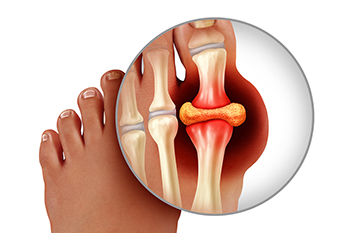
Chronic tophaceous gout is a severe stage of gout that impacts the feet, toes, and ankles, causing significant discomfort and potential joint damage. Chronic tophaceous gout occurs when uric acid levels remain consistently high, leading to the formation of tophi, which are hard, chalky deposits of urate crystals that form under the skin around joints and tissues. These tophi often appear as painful lumps that can contribute to swelling, redness, warmth, and tenderness in the affected areas, commonly the big toe or ankle. Left untreated, chronic tophaceous gout can lead to cartilage damage, bone erosion, and a decreased range of motion in the feet and ankles. Kidney issues, diabetes, or consuming a diet high in purine-rich foods can increase the likelihood of developing tophaceous gout. A podiatrist can identify tophi, offer guidance on lifestyle adjustments, and recommend treatment to control uric acid levels and minimize joint damage. If you are suffering from gout in your feet, it is suggested that you schedule an appointment with a podiatrist for an exam and treatment options.
Gout is a foot condition that requires certain treatment and care. If you are seeking treatment, contact Dr. Eddy Caldwell from Foot Care of Northeast Arkansas, P.A.. Our doctor will treat your foot and ankle needs.
What Is Gout?
Gout is a type of arthritis caused by a buildup of uric acid in the bloodstream. It often develops in the foot, especially the big toe area, although it can manifest in other parts of the body as well. Gout can make walking and standing very painful and is especially common in diabetics and the obese.
People typically get gout because of a poor diet. Genetic predisposition is also a factor. The children of parents who have had gout frequently have a chance of developing it themselves.
Gout can easily be identified by redness and inflammation of the big toe and the surrounding areas of the foot. Other symptoms include extreme fatigue, joint pain, and running high fevers. Sometimes corticosteroid drugs can be prescribed to treat gout, but the best way to combat this disease is to get more exercise and eat a better diet.
If you have any questions please feel free to contact our office located in Jonesboro, AR . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Everything You Need to Know About Gout
Gout, typically found in diabetic patients, is an unusually painful form of arthritis caused by elevated levels of uric acid in the bloodstream. The condition typically strikes the big joint on the big toe. It has also been known to strike the knees, elbows, fingers, ankles and wrists—generally anywhere that has a functioning, moving joint.
The high level of uric acid in a person’s bloodstream creates the condition known as hyperuricema—the main cause of gout. Genetic predisposition occurs in nine out of ten sufferers. The children of parents who suffer gout will have a two in ten chance of developing the condition as well.
This form of arthritis, being particularly painful, is the leftover uric acid crystallizing in the blood stream. The crystallized uric acid then travels to the space between joints where they rub, causing friction when the patient moves. Symptoms include: pain, redness, swelling, and inflammation. Additional side effects may include fatigue and fever, although reports of these effects are very rare. Some patients have reported that pain may intensify when the temperature drops, such as when you sleep.
Most cases of gout are easily diagnosed by a podiatrist’s assessment of the various symptoms. Defined tests can also be performed. A blood test to detect elevated levels of uric acid is often used as well as an x-ray to diagnose visible and chronic gout.
Treatment for gout simply means eliminating symptoms. Non-steroid anti-inflammatory drugs or NSAIDs (Colchicine and other corticosteroid drugs, etc.) will quell the redness, the swelling, and the inflammation. However, managing your diet, lifestyle changes, and using preventative drugs are all helpful toward fully combating the most severe cases.
Those that lead an inactive lifestyle are at a higher risk for gout. Any amount of exercise decreases the probability of repeat encounters with the condition. Reducing your consumption of red meat, sea food, and fructose-sweetened drinks also reduces the likelihood of chronic gout as well.
Ingesting Vitamin C, coffee, and particular dairy products can help with maintaining a healthy lifestyle. There are new drugs out on the market that inhibit the body’s production of uric acid-producing enzymes. However, reducing or eliminating your overall levels of uric acid is the best remedy to ensuring you lead a gout-free life.
Sources of Big Toe Pain

Big toe pain can stem from various conditions, including turf toe and sesamoid fractures, both of which are common in athletes. Turf toe is a sprain of the ligaments surrounding the big toe joint. It is typically caused by hyperextension of the toe during activities like running or football. Symptoms include pain, swelling, and limited movement in the big toe. A sesamoid fracture involves a break in the small bones called sesamoids, under the big toe joint. This injury is often caused by repetitive stress, sudden impact, or wearing improper footwear. Symptoms include localized pain, swelling, bruising, and difficulty bearing weight on the foot. Treatment for both conditions may involve rest, anti-inflammatory medications, and wearing a stiff-soled shoe or brace to limit toe joint movement. In severe cases, a podiatrist may recommend custom orthotics, targeted exercises, or surgery to promote healing. If you have toe pain, it is suggested that you schedule an appointment with a podiatrist.
Toe pain can disrupt your daily activities. If you have any concerns, contact Dr. Eddy Caldwell of Foot Care of Northeast Arkansas, P.A.. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Causes Toe Pain?
Most severe toe pain is caused due to a sports injury, trauma from dropping something heavy on the toe, or bumping into something rigid. Other problems can develop over time for various reasons.
Toe pain can be caused by one or more ailments. The most common include:
- Trauma
- Sports injury
- Wearing shoes that are too tight
- Arthritis
- Gout
- Corns and calluses
- Hammertoe
- Bunions
- Blisters
- Ingrown toenails
- Sprains
- Fractures (broken bones)
- Dislocations
When to See a Podiatrist
- Severe pain
- Persistent pain that lasts more than a week
- Signs of infection
- Continued swelling
- Pain that prevents walking
Diagnosis
In many cases the cause of toe pain is obvious, but in others, a podiatrist may want to use more advanced methods to determine the problem. These can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatments for toe pain and injuries vary and may include shoe inserts, padding, taping, medicines, injections, and in some cases, surgery. If you believe that you have broken a toe, please see a podiatrist as soon as possible.
If you have any questions please feel free to contact our office located in Jonesboro, AR . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.